5. EQUIPMENT AND PRODUCTS
5.1 Types of catheters
A catheter is a thin hollow tube that can be inserted in the bladder either through the urethra or suprapubically.
5.1.1 Balloon catheter or two-way catheter for suprapubic or transurethral catheterization
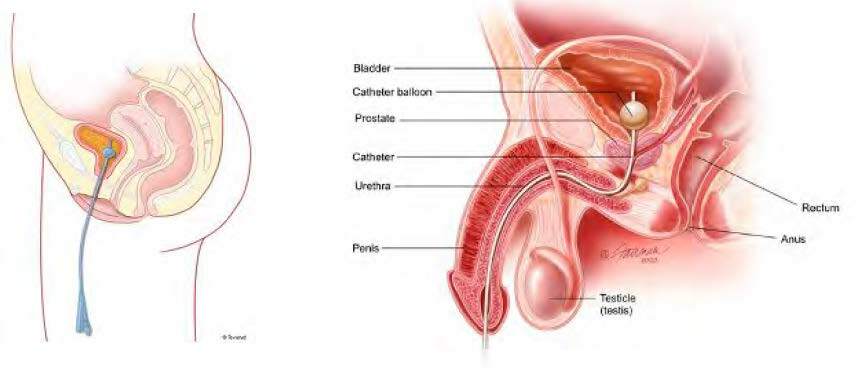
Left: Fig. 1 Female transurethral catheter
(Courtesy of Coloplast A./S, see chapter 15)
Right: Fig. 2 Male transurethral catheter
(Courtesy of Urologyhealth.org, see chapter 15)
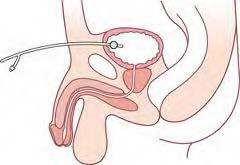
Fig. 4 Male suprapubic catheter
(Courtesy of Coloplast A./S, see chapter 15)
In 1853, Jean Francois Reybard developed the first indwelling catheter with an inflated balloon to secure its place in the bladder. One channel is used for urine and one for the balloon (Fig. 5). In 1932 Dr. Frederick Foley redesigned this catheter. The general name of the two-way urinary catheter is the Foley catheter.
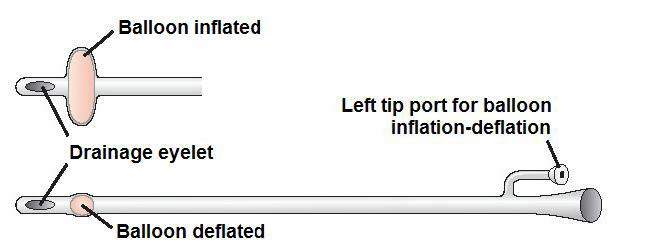
Fig. 5 Two-way catheter with an inflated and deflated balloon
(Courtesy of Essential Clinical Procedures, see chapter 15)
Indications for a two-way catheter:
- Standard transurethral catheterisation
- Standard suprapubic catheterisation
5.1.2 Integrated balloon catheter
The Fortune® integrated balloon catheter is designed to eliminate the uneven edge out of an ordinary balloon. The balloon is integrated into the catheter shaft to create a complete smooth surface with the aim to reduce friction, trauma, discomfort and accumulation of urine sediment. It can be used transurethral and suprapubic (2-way catheter).

Fig. 6 Balloon catheters. Left: ordinary balloon; right: integrated balloon
(Courtesy of Fortune Medical, see chapter 15)
5.1.3 One-way suprapubic catheter
The one-way suprapubic catheter has no balloon and requires a suture to the skin to secure in place.
Indications for a suprapubic one-way catheter:
- Alternative to the suprapubic catheter with balloon
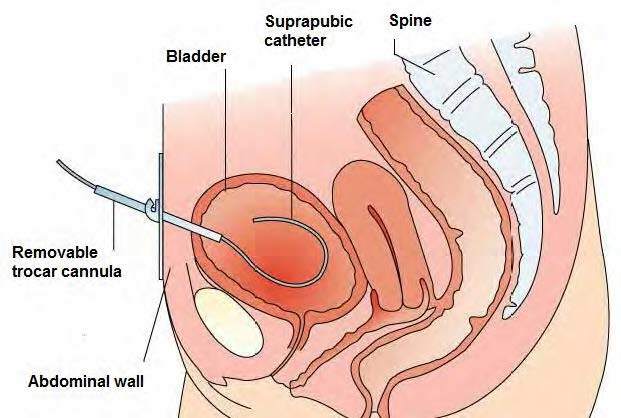

Fig. 3 Suprapubic catheter without a balloon
(Courtesy of Hospital Santa Maria Lleida)
Catheter with open-end tip
A catheter with an open end has no “eyes” but an open-end tip and is referred to as a “council” tip. This type of catheter can be used when changing a fine-bore suprapubic catheter to a suprapubic long-term catheter and when changing a long-term suprapubic catheter – usually performed using a guide wire.

Fig. 7 From left to right: Straight catheter with rounded tip with one eye, rounded tip with two eyes, open end tip
(Courtesy of V. Geng)
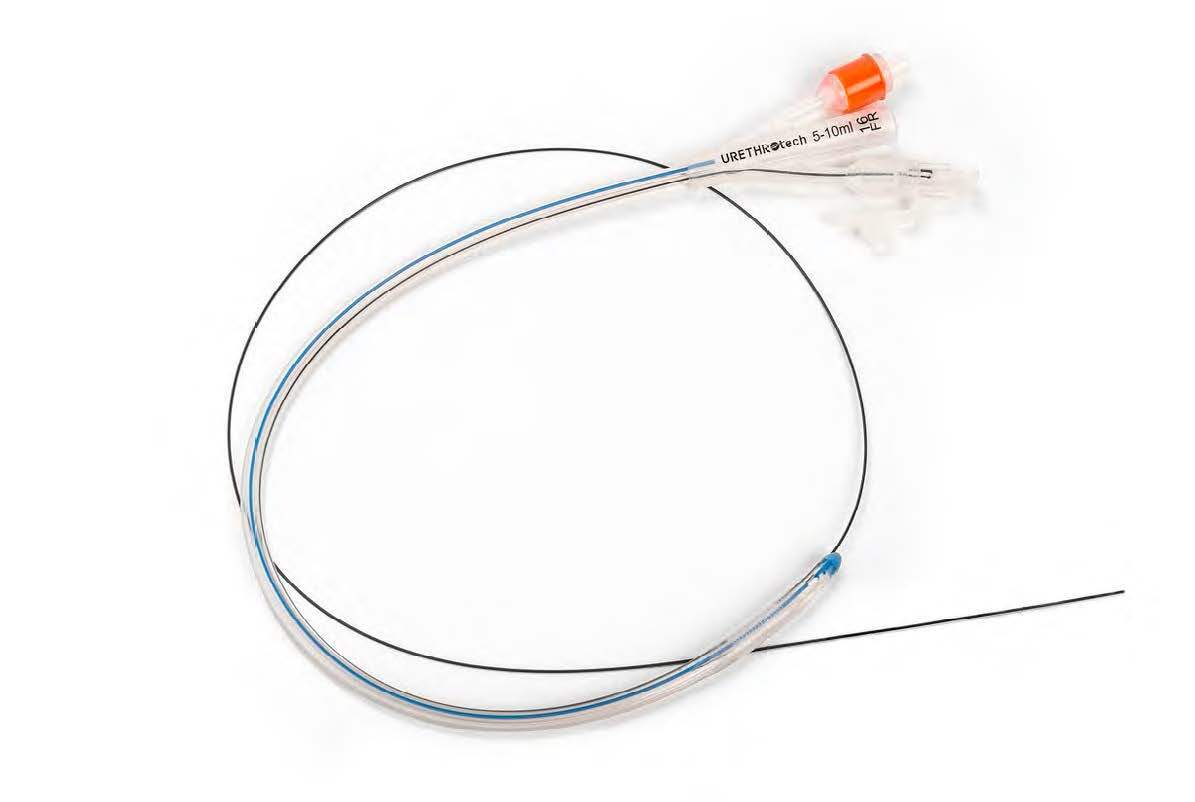

Fig. 8 Transurethral catheter with guidewire for difficult catheterisation
Urethral catheterisation device (UCD)
(Courtesy of Urethrotech, see chapter 15)
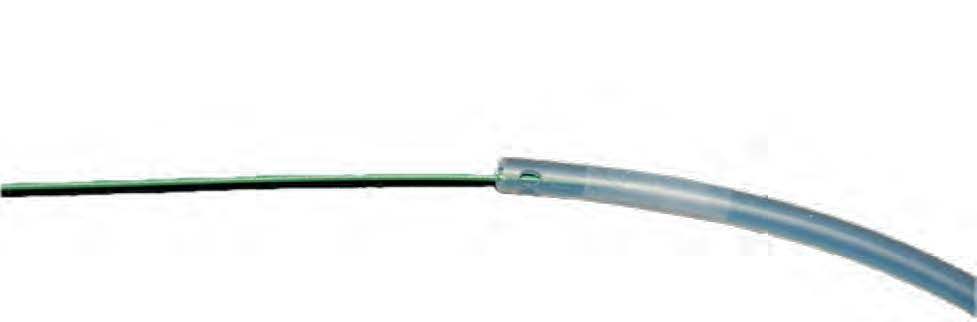

Fig. 9 Open-end catheter with a guide wire (close-up picture where the
guide wire enters the catheter)
(Photo courtesy of T. Schwennesen)
5.1.4 Three-way catheter
Three-way catheters are available with a third channel to facilitate continuous bladder irrigation.

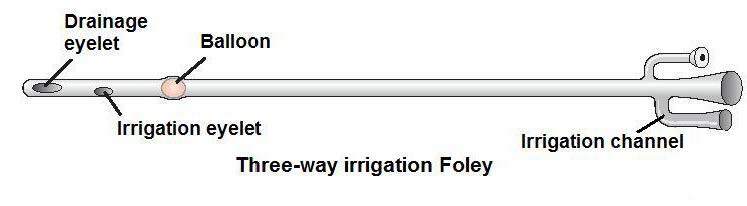
Fig. 10 Three-way catheter with irrigation channel
(Courtesy of: Essential Clinical Procedures, see chapter 15)
Indications for three-way catheterisation:
- Following urological surgery to perform continuous irrigation
- Bladder washout/irrigation to clear blood clots or debris
5.2 Catheter material characteristics
Catheters are available in various materials. Some aspects that should be considered when choosing a catheter are indication, allergy (latex), tissue compatibility, tendency for encrustation and biofilm formation, patient comfort and ease of use. Some manufacturers produce catheters without phthalates and polyvinyl chloride (PVC) because PVC includes chlorine and plasticisers, which are environmentally hazardous.
5.2.1 Types of material and coating
| Catheter material/coating | Advantages | Disadvantages | Recommended use |
| Latex | Flexible Cheap | Not suitable for people with latex allergy More risk of irritation | Short-term < 14 days |
| Silicone | Wider lumen than latex Less encrustation Suitable for people with latex allergy May reduce mucosal encrustation | Less flexible Balloon may shrink due to fluid loss through diffusion | Long-term > 14 days |
| Hydrogel-coated latex | May reduce friction during insertion May reduce encrustation | Not suitable for people with latex allergy | Long-term > 14 days |
| Silicone-coated latex | Flexibility between latex and pure silicone Biocompatibility of silicone and flexibility of latex | Not suitable for people with latex allergy | Long-term > 14 days |
| PTFE (Teflon)-coated latex | Prevents encrustation and irritation | Not suitable for people with latex allergy | Long-term > 14 days |
| Nobel alloy-coated | Reduces biofilm-formation | May be more expensive | Short-term < 14 days |
| Nitrofurazone-coated | Antimicrobial | No clear statement about antibiotic resistance identified | Short-term < 14 days |
Latex
Latex made from natural rubber is a flexible material, but it has some disadvantages. The use of latex catheters is restricted to short-term indwelling catheterisation and is avoided if possible because of the potential discomfort due to high surface friction, vulnerability to rapid encrustation by mineral deposits from the urine, and the implication of latex allergic reactions in the development of urethritis and urethral stricture or anaphylaxis. [8]
Silicone
The silicone catheter (100% silicone) is gentle on tissue and is hypoallergenic, because it is uncoated. Catheters formed of silicone material have a relatively large lumen that reduces the tendency to encrustation.
While silicone catheters cause less tissue irritation and potential damage than latex or latex-coated catheters, the catheter balloon tends to lose fluid. A scoping review of urinary catheter induced complications reported, that the tendency to lose fluid increases the risk of displacement.
Silicone catheters also have a greater risk for developing a cuff when deflated that can result in uncomfortable catheter removal or urethral trauma. [42]

Fig. 11 Removed catheter with a cuff (folded due to incorrect deflation)
(Photo courtesy of S. Vahr Lauridsen)
A Cochrane review from 2012 did not find sufficient evidence to determine the best type of indwelling urinary catheter for long-term bladder drainage in adults. [43] However, silicone might be preferable to other catheter materials to reduce the risk of encrustation in long-term catheterised patients.
Latex with silicone or silicone elastomer-coating
Silicone elastomer-coated catheters are latex catheters coated inside and out with silicone. The catheter has the strength and flexibility of latex and the durability and reduced encrustation typical of 100% silicone catheters. [44]
Latex with polytetrafluoroethylene (PTFE)-coating
PTFE-coated latex (commonly known as Teflon) catheters have been developed to protect the urethra against latex. The absorption of water is reduced due to the Teflon coating. It is smoother than plain latex, which helps to prevent encrustation and irritation. These catheters should not be used for patients who are latex sensitive. [45, 46]
Hydrogel-coating
Hydrogel-coated catheters are soft and biocompatible. Because they are hydrophilic, they absorb fluid to form a soft cushion around the catheter, and reduce friction and urethral irritation. [44]
Nobel alloy-coating
- Silver alloy / silver alloy layer/ silver oxide layer
- Palladium
- Gold
The nobel alloy-coated catheters are not antiseptic-coated, but the metal in the coating creates a galvanic effect which reduces biofilm-formation.
Silver alloy-coated catheters significantly reduce the incidence of asymptomatic bacteriuria, but only for < 1 week. There is some evidence of reduced risk for symptomatic urinary tract infection (UTI). Therefore, they may be useful in some settings. [6, 18, 47]
Silver oxide-coated catheters are not associated with a significant reduction in bacteriuria. [8, 39, 43]
Nitrofurazone-coating
Catheters coated with nitrofurazone are also available. Nitrofurazone should be distinguished from the drug nitrofurantoin. Nitrofurazone is a bactericidal compound that is used as an antibiotic.
Comparisons
Antimicrobial‐impregnated (nitrofurazone-coated) versus antiseptic-coated (silver alloy) or standard PTFE-coated latex indwelling urethral catheters.
The evidence suggests that antimicrobial‐impregnated catheters do slightly reduce CAUTI in hospitalised adults catheterised short‐term. They also reduce bacteriuria to a significant degree. However, they are associated with greater patient‐reported discomfort. Whilst these catheters may be cost‐effective, it remains unclear if the marginal benefits are clinically important. Some uncertainties also remain over how beneficial the catheters are beyond one week of catheterisation. [6]
Antiseptic-coated and standard PTFE-coated latex show no significant difference in symptomatic CAUTI. [43]
Potential toxicity and antibiotic resistance using antimicrobial catheters are unknown. [8]
Silicone versus silicone-coated catheters
After 5 days of indwelling catheterisation, pure silicone catheters have significantly less bacterial colonisation than silicone-coated latex catheters have (p = 0.03) and the biofilm formation of colonising bacteria is also significantly less with the pure silicone catheter (p = 0.02). [48]
For selection of the most suitable material, the specifications of the supplier can be helpful.
| Recommendations | LE | GR |
| Use silicone catheter material for long-term catheter use. [49] | 1a | A |
| Use latex catheter material for short-term catheter use, unless the patient has a latex allergy. [49] | 1a | A |
| Silver alloy-coated catheters may slightly reduce the risk of catheter-associated bacteriuria in hospitalised patients during short-term catheterisation (< 1 week) [6, 18] | 1a | B |
| Antibiotic-impregnated catheters slightly decrease the frequency of CAUTI and significantly decrease asymptomatic bacteriuria in hospitalised patients within 1 week compared to silver alloy‐coated (antiseptic‐coated) catheters. [6] | 1a | B |
5.2.2 Diameter and length
Catheter diameter is measured in Charrière (Ch or CH) also known as French Gauge (F, Fr or FG) and indicates the external diameter. 1 mm = 3 Ch and the sizes range from Ch 6 to 30.
| Patient group | Urine characteristics | Catheter size |
| Paediatric | 6–10 | |
| Adult, with very small body size | Clear urine, no debris, no grit (encrustation) | 10 |
| Adult | Clear urine, no debris, no grit, no haematuria | 12-14 |
| Adult | Slightly cloudy urine, light haematuria with or without small clots, none or mild grit, none or mild debris. | 16 |
| Adult | Moderate to heavy grit, moderate to heavy debris. | 18 |
| Haematuria with moderate clots. | 18 | |
| Adult | Heavy haematuria, need for flushing [50] | 20-24 |
The size of the catheter is marked at the inflation channel as well as with an (international) colour code. (Fig. 12)
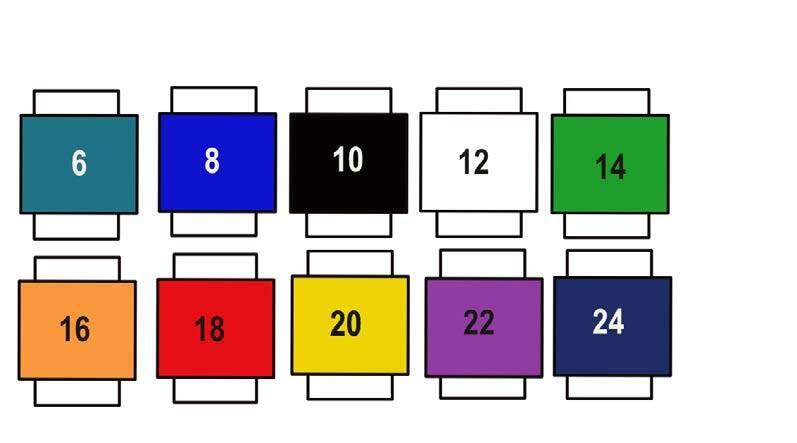
Fig. 12 International colours of catheter size
(Courtesy of V. Geng)
The inner lumen of the catheter varies between different catheter materials; e.g., latex and silicone, so inserting a larger Charrière catheter does not necessarily ensure a wider drainage channel. [51] (Fig. 13)
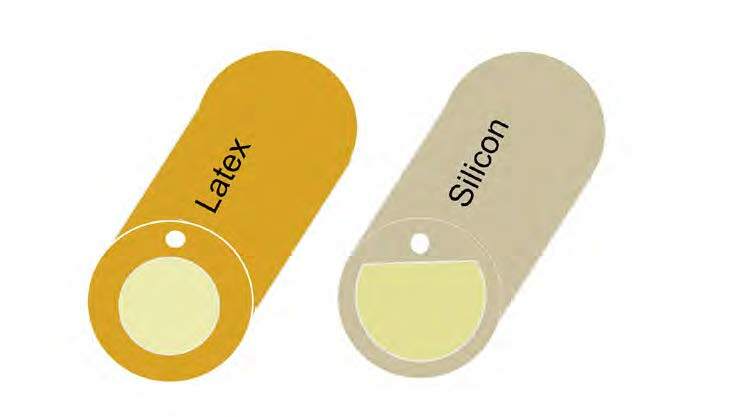
Fig. 13 Examples of silicon and latex catheter lumen
(Courtesy of V. Geng)
The standard male catheter length of 41–45 cm can be used for men and women, but a shorter female length of 25 cm can be more comfortable and discrete for some women. However, a female catheter can be too short if the woman is severely obese and thus a male length is preferable.
The female length catheter should not be used for men as inflation of the balloon within the urethra can result in severe trauma. Paediatric catheters are normally about 30 cm long. [8]
| Recommendations | LE | GR |
| Use the smallest bore catheter possible consistent with good drainage, to minimise bladder neck and urethral trauma, unless otherwise clinically indicated [24] | 1b | B |
| Use male standard length for female patients who are bedbound, immobile, clinically obese with fat thighs, critically ill and postoperative and in emergency situations [16] | 4 | C |
| Do not use the female length catheter for males in urethral catheterisation as inflation of the balloon within the urethra will result in severe trauma. [8] | 4 | A |
5.2.3 Tip design
There is a wide variety of catheter tips. The two main tips are the straight tip and coudé tip. Coudé is French and means a catheter which is bended slightly at the tip.
Straight tip (Nelaton tip)
A catheter with a standard round tip with drainage eyes is called a Nelaton catheter. (Fig. 14) For routine catheterisation, a straight-tipped catheter should be used. [44]
Bended tip (coudé tip)
There are three different coudé tip designs:
Tiemann
The Tiemann catheter with the curved tip is designed to negotiate the male prostatic curve and can be helpful for difficult insertions. [44]
Olive tip
The olive tip is a little larger than a standard tip but the circular shape allows to widen narrow urethras. The rounded end helps to avoid to get stuck in any obstruction.
Tapered tip
The tapered tip catheter has a curved tip just like the Tiemann catheter but has one, two or three drainage eyes situated in the curved tip.
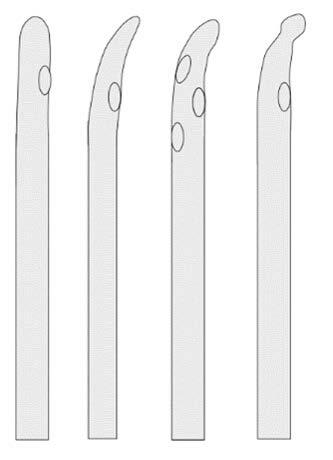
Fig. 14 From left to right: Nelaton tip, Tiemann tip, tapered tip and olive tip
(Courtesy of V. Geng)
| Recommendations | LE | GR |
| For routine catheterisation, a straight-tipped catheter should be used | 4 | C |
| The coudé tip catheter can be used where male catheterisation is complicated and should be inserted with the tip pointed upward (dorsally) | 4 | C |
5.2.4 Balloon size and filling
When the catheter has been placed in the bladder, the balloon can be inflated according to the instructions of the manufacturer. To make sure the catheter is not inflated in the urethra, insert the catheter until the hub/bifurcation before filling the balloon, especially in men.
Sterile water or sodium chloride can be used for latex catheters. Inflation of silicone catheters with water can lead to water loss from the balloon over time, with an associated risk of the catheter falling out. Some manufacturers recommend filling the balloon with a 10% aqueous glycerine solution. [8]
Huang et al. demonstrated in an in vitro equivalence study that there was no difference in filling the balloon with water, glycerine or saline in the rates of balloon deflation failure. [52]
Some catheter manufacturers provide sterile pre-filled syringes with sterile water or 10% glycerine inside the packaging.
The balloon volume is indicated at the catheter connection behind the size of the catheter as a minimum and maximum; e.g., Charrière 12/5–10 ml or cc (cm3).
In special situations, special catheter designs are available e.g., haematuria catheter. The volume of the catheter balloon can differ and the manufacturer’s instructions should be followed. [44]
A catheter with a 30 ml balloon is designed specifically as a haemostat post urological procedure, and should not be used for routine catheterisation.
The purpose of the retention balloon is to keep the catheter in place in the bladder. The use of a larger balloon size is mistakenly believed to be a solution to bypassing urine. [51] However, increasing the amount of fluid in the balloon may increase the risk of pressure ulcer at the bladder neck and will not solve the problem of leak of urine around the outside of the catheter. (see Section 7.5 Catheter bypassing).
Under- or overinflation can cause occlusion of drainage eyes, irritate the bladder wall, and lead to bladder spasms. [44]
Large balloons tend to sit high in the bladder, with potential for increased residual urine volumes to collect below the catheter eyes. [8]
Some manufacturers have catheters with an integrated balloon, which means that the balloon is at the same level as the catheter when it is deflated. It can be an advantage when removing a catheter with encrustations because the encrustations are gathered around the deflated balloon cuff.
| Recommendation | LE | GR |
| Always inflate the balloon according to the manufacturer’s instructions | 4 | C |
5.3 Catheter sets
Different types of catheter sets are available for indwelling and suprapubic catheterisation (refer to local policy). There is no standard list of materials for a catheterisation set/pack. A catheter set could contain gloves, underlay, cotton balls and gauzes, forceps, and aperture drape for the preparatory stage of catheterisation. It also provides the lubricating gel for the introduction of the urinary catheter and sterile water for inflating the balloon of a self-retaining Foley catheter. One should check individual packs for required contents; the catheter and drainage bag are usually separate from the catheterisation packs.
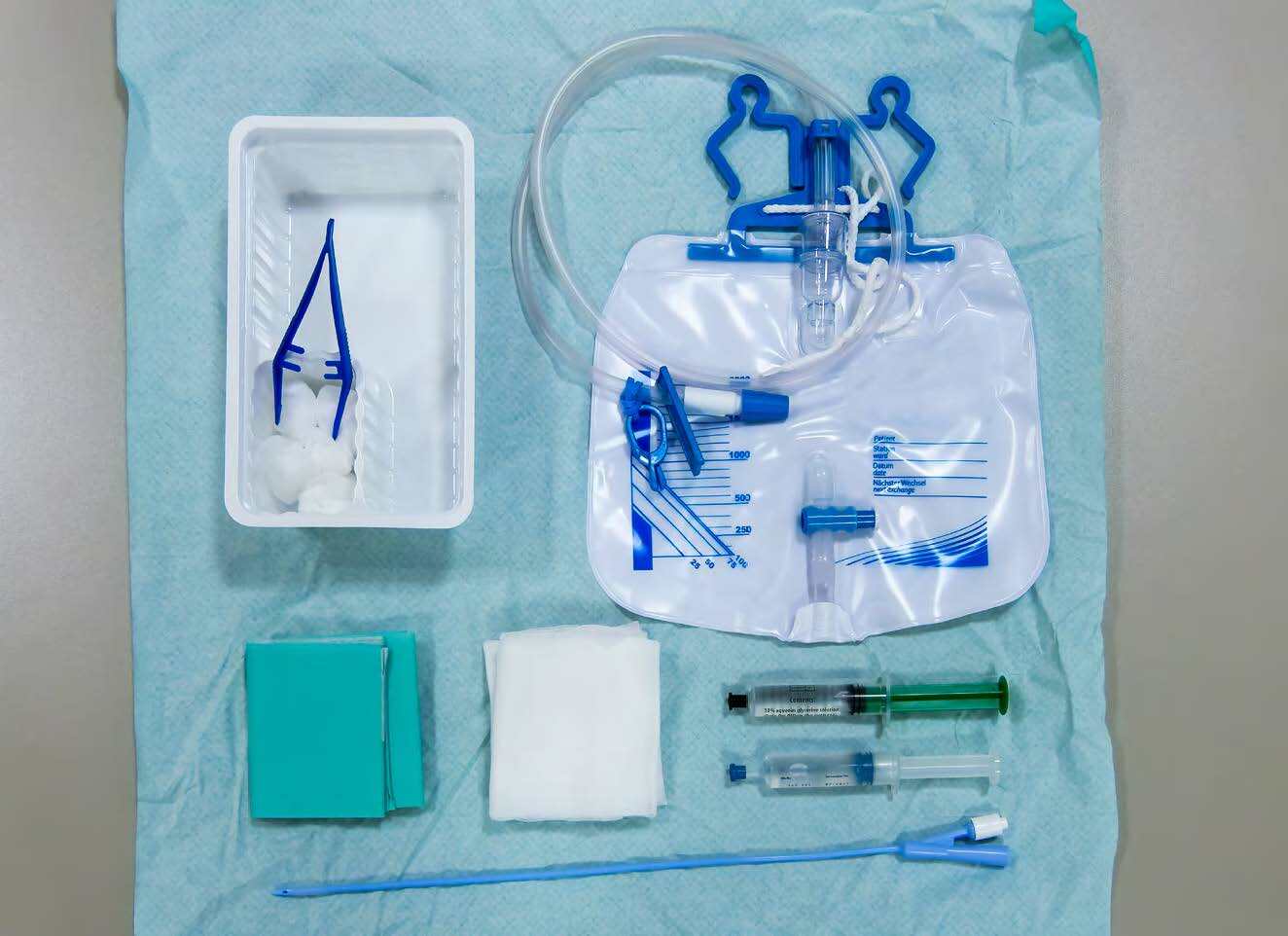
Fig. 15 Catheter set with Foley catheter
(Photo courtesy of P. Wenig)
Also sets for suprapubic application are available; for example, a catheter with insertion trocar and plug (spigot) (Fig. 16).
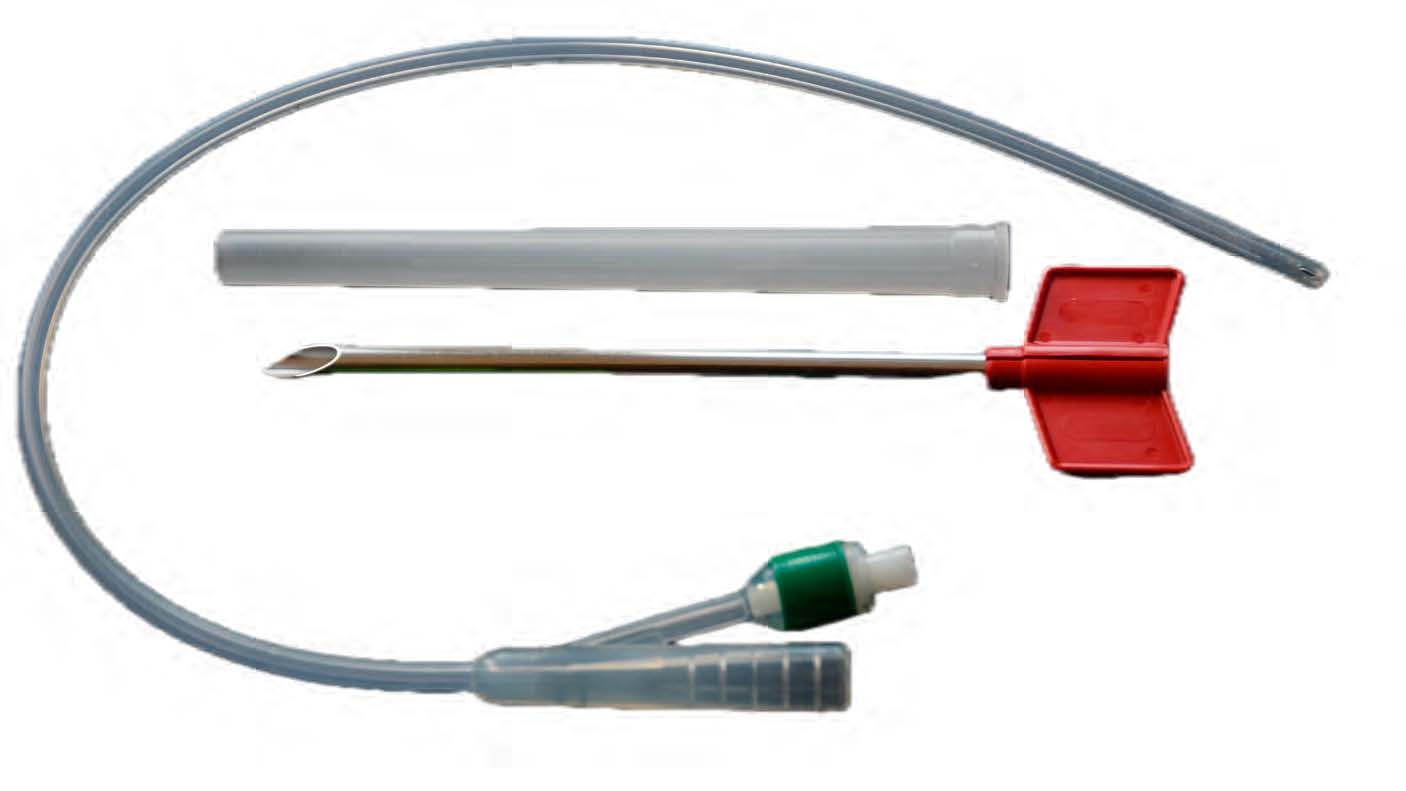
Fig. 16 Catheter set to insert a suprapubic catheter
(Photo courtesy of T. Schwennesen)
The purpose of using catheter sets is to prevent unwanted variation in clinical practice and to save time finding all the items used for catheterisation. Two quality improvement studies have evaluated the effect of implementing urinary catheter sets together with an education and training programme and found an 80% reduction in CAUTI after 1 year. [53, 54] (LE 4)
5.4 Drainage bags
5.4.1 Closed drainage system
When a catheter is inserted using aseptic technique, it is directly connected to the sterile bag, because an aseptic closed drainage system minimises the risk of catheter-associated urinary tract infection. [55] Unnecessary disconnection of a closed drainage system should be avoided [56], but if it occurs, the catheter and collecting system must be replaced using aseptic technique and sterile equipment. [24]
There are several different bags available; selection of the bag depends on whether it is for short-term drainage at the hospital or for long-term use, the patient’s mobility, cognitive function, daily life etc. The bags can have a variety of special features.

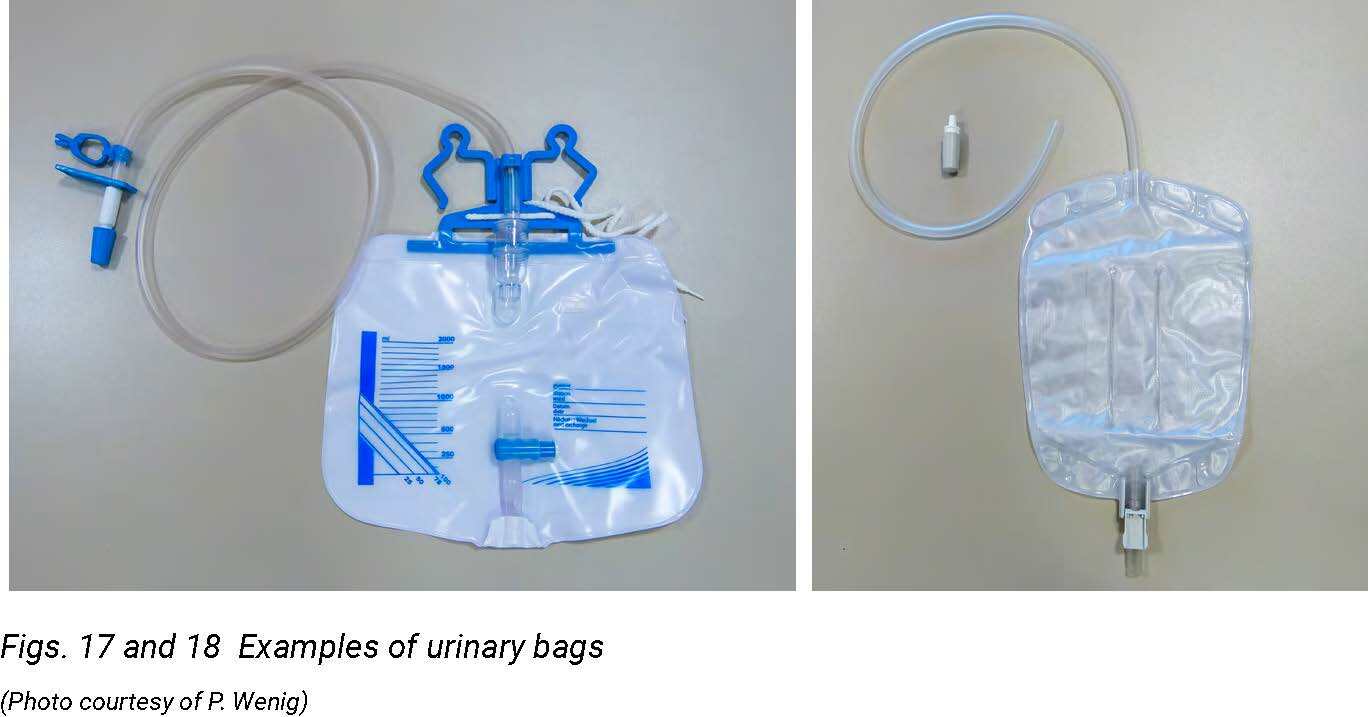
Figs. 17 and 18 Examples of urinary bags
(Photo courtesy of P. Wenig)
Pre-connected drainage systems are available in which the drainage bag is already connected to a catheter in a sterile pack and a tamper-evident seal protects the connection. The use of urinary systems with pre-connected, sealed catheter–tubing junctions may reduce the occurrence of disconnection. [19, 24]
Anti-reflux valve drainage bags are designed with either an anti-reflux valve or chamber to prevent reflux of contaminated urine from the bag into the tubing. [44] However, complex urinary drainage systems (utilising mechanisms for reducing bacterial entry such as antiseptic-release cartridges in the drain port) are not necessary for routine use. [24]

Fig. 19 Drainage bag with anti reflux dome
(Photo courtesy of P. Wenig)
Sampling port: most drainage bags have a special sampling port designed to obtain urine specimens while maintaining a closed system. (Fig. 20) Some companies produce bags with a needle-free sampling port to avoid sharp injury.
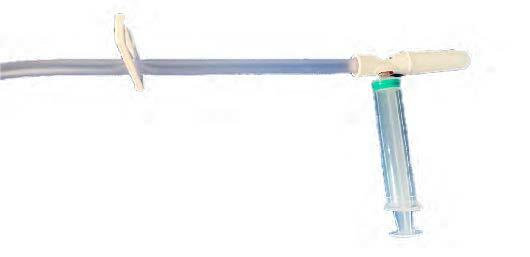
Fig. 20 Collection of a catheter specimen of urine – needle free
(Photo courtesy of S. Vahr Lauridsen)
5.4.2 Large capacity bag
Large capacity bags (2–4 l) can be used postoperatively, if the patient is confined to bed or if the use of a leg bag is not appropriate. Some of the large-capacity bags are provided with a urometer which allows accurate measurement of urine in intensive care patients.

Fig. 21 Drainage bed bag with urine meter
(Dover Precision Urine Meter, Courtesy of Cardinal Health, see chapter 15)
Different outlet taps and tube lengths are available as for leg bags (see Section 5.4.3).
5.4.3 Leg bag/body worn urine collection bag
If the patient is mobile a leg bag can be preferable. A leg bag allows maximum freedom and movement and can be concealed beneath the clothes.
Leg bags are available in different sizes (120–1000 ml), designs and qualities and it is important to select a bag and a bag length according to the patient’s preference and mobility and the intended duration of use. (Fig. 22)

Fig. 22 Different types of leg bags
(Photo courtesy of T. Schwennesen)
Another discreet bag that allows mobility is the body-worn bag; e.g., the Belly Bag® (Fig. 23). The bag can be used with either a suprapubic, urethral or nephrostomy catheter, but is not intended to be used with a male external catheter (condom or urosheath) in men. An anti-reflux valve behind the catheter port prevents reflux urine flow, which allows positioning of the bag above the level of the bladder, contrary to other bags. It is not intended to be used permanently, but for short-term use; e.g., during sports or when visiting a sauna.
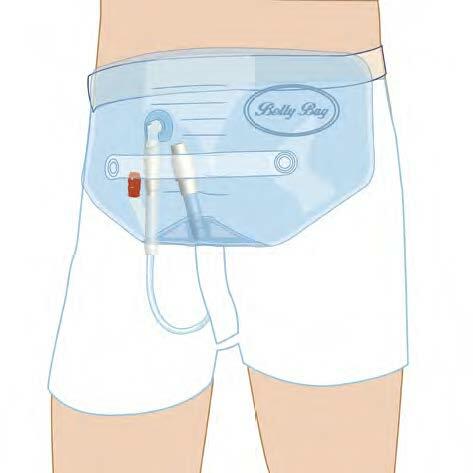
Fig. 23 Body worn bag
(Courtesy of Teleflex Europe Ltd., see chapter 15)
Capacity: ranges from 120 to 1000 ml and the size depends on how often the bag has to be emptied, according to the patient’s daily routines.
Chamber: the bags are available with a single or several chambers. Several chambers flatten the bag’s profile and are therefore more discreet.
Materials: bags are produced in different materials with different backings and comfort. Some of the bags are PVC free as well.
Tube: ranges from 4 to 45 cm and some can have an individual length by cutting the tube. Some tubes are kink free, which reduces the risk of obstruction.

Fig. 24 Anti-kinking collection bag tubing
(Courtesy of Continence Product Advisor, see chapter 15)
Suspension system: leg bags can be attached to the leg with straps (elasticated), nets, bags/pockets of cotton, etc. (Fig. 25)
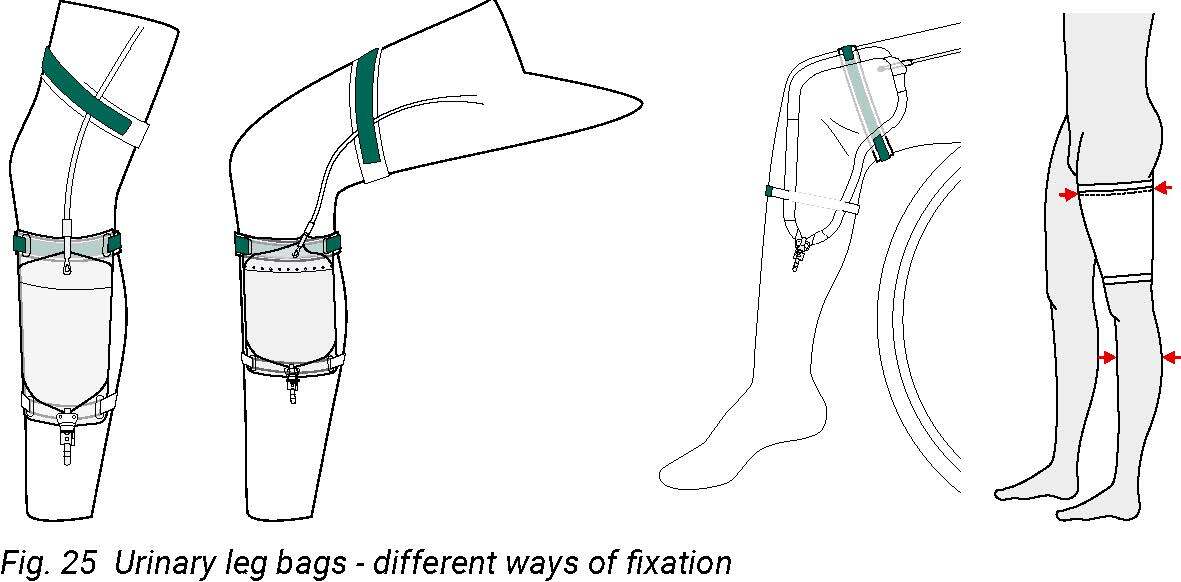
Fig. 25 Urinary leg bags - different ways of fixation
(Courtesy of Manfred Sauer GmbH, see chapter 15)
Outlet tap: is available in different designs: barrel tap, lever tap and push–pull tap. [51] It is important to choose a bag with a tap that the patient can manage, especially in patients with reduced hand function. (Figs. 26, 27)
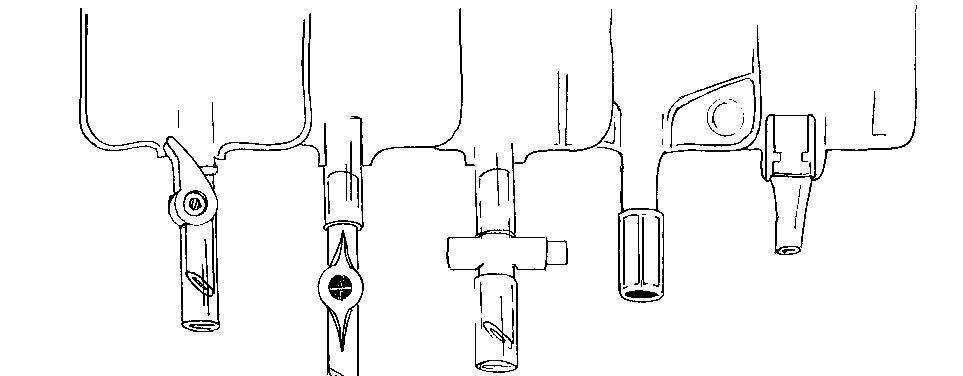
From left to right: Lever tap; t tap; cross valve; push-pull tap
Fig. 26 Examples of bag taps
(Courtesy of ICUD, see Chapter 15)

Fig. 27 Quadriplegic patient with poor manual dexterity
(Courtesy of T. Schwennesen)
(Please note that the bag is being held above the level of the bladder for photographic purposes only)
5.4.4 Combination of leg bag and overnight/bedside bag
Large capacity bags can also be used as overnight bags. Patients normally require a 2 l drainage bag that is connected to the leg bag at night or if they are immobile/bedbound.
The outlet tap on the leg bag is left open so that the urine collects in the larger bag without breaking the closed drainage system. [57] (Fig. 28)
The night bag requires a stand for support, to reduce the risk of dislodging the link system and is available in different designs and materials. [51]
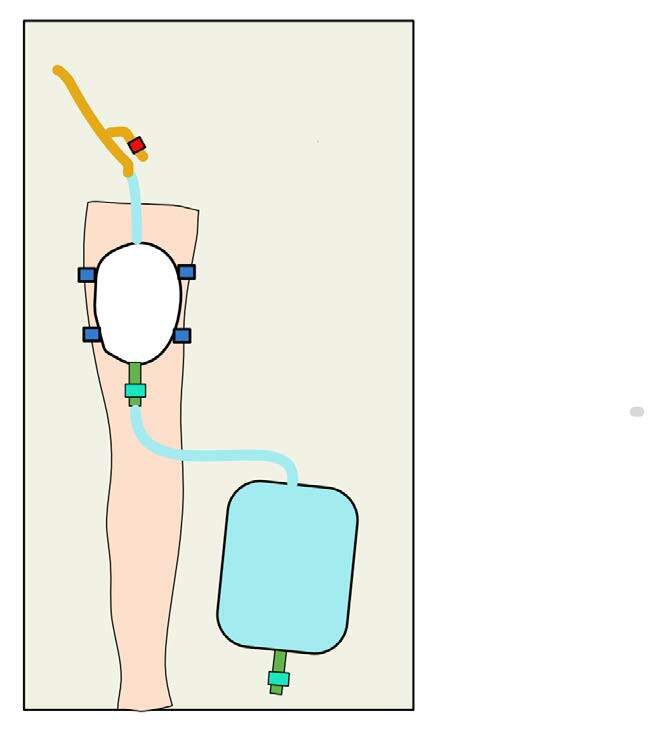
Fig. 28 Overnight drainage system
(Courtesy of V. Geng)
5.4.5 Single use urinary bag
It is common practice to use a sterile technique for short-term use and a clean technique for long-term use in the home care setting.
In some countries clean, single-use, non-drainable night bags are used, which means that when the bag is full, it has to be changed since the bag cannot be emptied. In other countries, night bags are cleaned and reused for long-term catheters at home. More research is needed to ensure that guidelines and resultant care are based on existing evidence rather than on custom and common practice. [10]
| Recommendations | LE | GR |
| A closed drainage system should be maintained to reduce risk of CAUTI [18, 24] | 3 | A |
| Unnecessary disconnection of a closed drainage system should be avoided, but if it occurs the catheter and collecting system have to be replaced using aseptic technique and sterile equipment [10, 24] | 3 | A |
| Complex urinary drainage systems (utilising mechanisms for reducing bacterial entry such as antiseptic-release cartridges in the drain port) are not necessary for routine use [24] | 3 | B |
| In selecting urinary drainage bags, attention should be focused on: the ability of the user to operate the tap, comfort, freedom from leakage, and discretion [8] | 4 | C |
| Using a catheter set could reduce the risk of CAUTI [53, 54] | 3 | C |
| The patient’s individual needs and personal preferences should determine the kind of leg bag/suspension/ attachments and position of where the bag is worn [8] | 4 | C |
| Consult national policies for working with medical devices – and reuse of single-use material | 4 | C |
5.5 Valves
Valves are small devices connected to the catheter outlet instead of a bag and are available in a variety of designs. (Fig. 29)

Fig. 29 Different catheter valves
(Photo courtesy of T. Schwennesen)
The catheter valves are an alternative to leg bags/body-worn bags that give the patient more freedom to move and more discreet drainage. Most valves are designed to fit with linked systems so it is possible to connect to a drainage bag. For example, at night-time and for journeys. [51]
The valves provide a well-accepted system of bladder emptying for suitable patients who are able to manipulate the valve mechanism and empty the bladder regularly to avoid overfilling. An in vitro bladder model showed that using a catheter valve with a 2-4-hourly release was associated with reduced catheter blockage. [58] A randomised controlled trial from 2015 showed that the incidence of bacteriuria was not significantly lower in the non-return catheter valve group than in the simple urine bag group. [59]
Use of this urinary catheter valve increases patient satisfaction without affecting the postoperative UTI rate. This easy and inexpensive device could help patients have a better catheter experience and should be considered in women being discharged home with a urinary catheter. [60]
The valve is not an optimal solution for all patients, especially those with poor bladder compliance due to possible upper tract deterioration, and nurse specialists need to assess the suitability for each patient. However, in some countries the use of catheter valves is not approved.
The catheter valve is contraindicated in patients with:
- Urological surgery requiring an empty bladder postoperatively (prostatectomy, nephrectomy with removal of ureter and in case of bladder perforation)
- Short time catheter use postoperatively (to relieve pressure on the bladder)
- A risk of upper tract deterioration (patients with poor bladder compliance)
- Severe cognitive impairment (the patient must be able to recognise the need to empty the bladder through sensation or on a timed schedule)
- Overactive bladder syndrome; might cause urinary leakage
- Ureteral reflux or renal impairment
- Small or limited bladder capacity; the valve would have to be opened often
- UTI
- Poor manual dexterity [61]
Transurethral catheter safety valve
0.3-0.7% of hospitalised patients with an indwelling catheter will suffer a catheter balloon injury. [62]
The transurethral catheter safety valve prevents the risk of urethral catheter balloon injury. The device is designed to prevent inadvertent inflation of the catheter’s anchoring balloon in the urethra during urethral catheter insertion. The safety valve allows fluid in the catheter system to vent through a pressure relief valve if attempted intraurethral inflation of the catheter’s anchoring balloon occurs. [63]

Fig. 30 Transurethral catheterisation safety valve (TUCSV)
(Courtesy of Class Medical, see chapter 15)
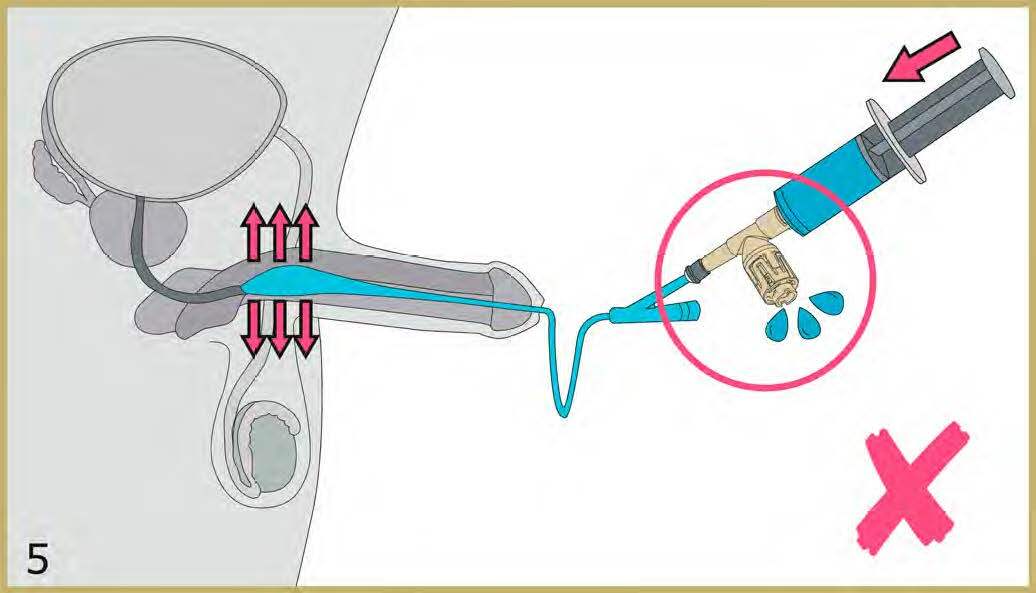
Fig. 31 Transurethral catheterisation safety valve venting (fluid leak) and signaling the
user when the balloon has been inadvertently inflated in the urethra
(Courtesy of Class Medical, see chapter 15)
| Recommendations | LE | GR |
| Suitability for catheter valves should be assessed by a health care professional | 4 | C |
| Catheter valves are non-inferior for bladder emptying for suitable patients who are able to manipulate the valve mechanism and empty the bladder regularly [60] | 1b | A |
| Combination of a valve during the day and free drainage at night through an open valve connected to a drainage bag could be an appropriate management strategy [8] | 4 | C |
| Implement a 2-4-hourly release if catheter valve is used [58] | 2a | B |
5.6 Securement devices
Catheter securement devices are designed to prevent excessive traction of the catheter against the bladder neck or inadvertent catheter removal. There are different kinds of securement devices such as tape, Velcro™. (Figs. 32, 33)
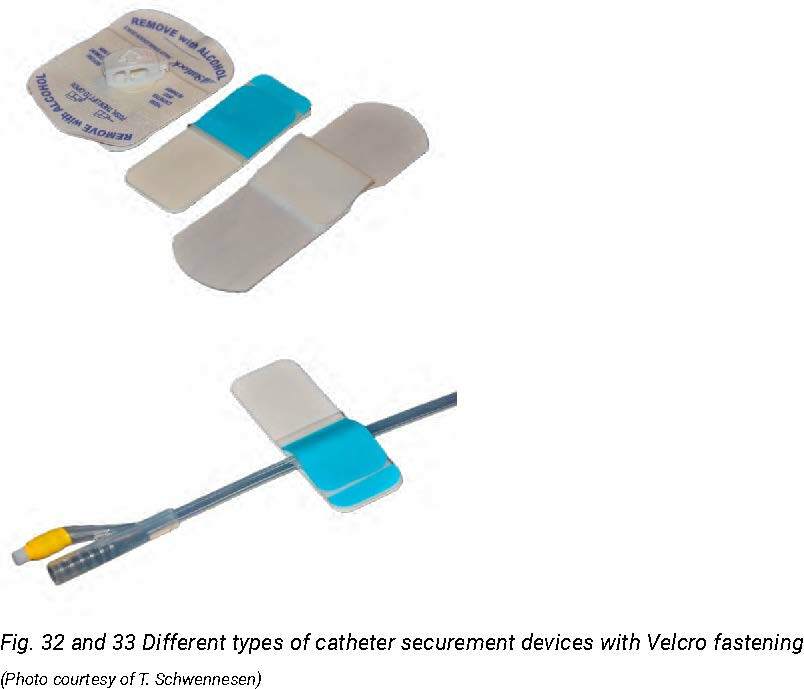
Fig. 32 and 33 Different types of catheter securement devices with Velcro fastening
(Photo courtesy of T. Schwennesen)
For more information about catheter securement see Section 6.5.3 Stabilising of the urethral catheter.
5.7 Lubricating gel
The lubricant dilates and lubricates the urethra. The lubricant does not need to be antiseptic or anaesthetic. [64]
Four types of lubricants can be distinguished:
- Water soluble
- Water soluble with chlorhexidine (antiseptic)
- Water soluble with anaesthetic lignocaine/lidocaine
- Water soluble with anaesthetic lignocaine/lidocaine and chlorhexidine
