15. INTERMITTENT URETHRAL DILATATION
Strictures are more common in men because the male urethra is longer than the female and the female urethra is straighter than the male. Urethral strictures/stenosis can occur due to:
- infection
- trauma
- catheterisation – indwelling and intermittent
- intra-urethral diagnostics and surgery
- radiotherapy
- congenital abnormalities
- inflammation
- putting foreign objects in the urethra
In addition to the above, the cause can be unknown. [11]
Identifying the cause of strictures can help treatment options to prevent occurrence of strictures and help to decrease iatrogenic causes. [196]
Table 13. European Association of Urology classification according to degree of urethral narrowing
| Category | Description | Urethral lumen (French [Fr.]) | Degree |
| 0 | Normal urethra on imaging | – | – |
| 1 | Subclinical strictures | Urethral narrowing but ≥ 16 Fr | Low |
| 2 | Low-grade strictures | 11–15 Fr | |
| 3 | High-grade or flow-significant strictures | 4–10 Fr | High |
| 4 | Nearly obliterative strictures | 1–3 Fr | |
| 5 | Obliterative strictures | No urethral lumen (0 Fr) |
15.1 Indications
- Urethral stricture disease
- Stenosis of the external urethral meatus
- Bladder outflow obstruction
- Incomplete bladder emptying
- Inability to void
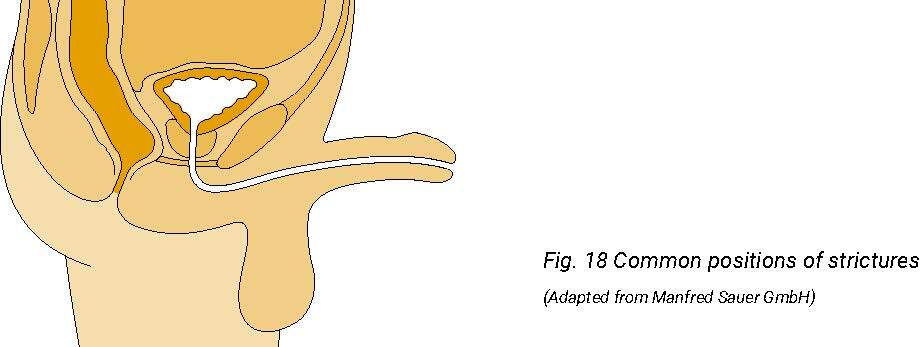

Fig. 18 Common positions of strictures
(Adapted from Manfred Sauer GmbH)
Left: Meatal stenosis/stricture
Middle: Strictures of the urethra
Right: Bulbar urethral stricture
15.2 Contraindications
- Suspected or confirmed urethral rupture
- Suspected or confirmed urinary tract infection
- Suspected or confirmed false passage
A urethral stricture can result from any process that causes injury to the urethral epithelium and then lead to scarring during the healing process and subsequent formation of a stricture. Urethral strictures predominantly occur in males causing obstructive voiding symptoms.
Urethral strictures are common and can be a result of intermittent catheterisation (IC) [80] or other causes: infection, trauma, lichen sclerosus, post-prostate cancer treatment (e.g., radiotherapy), or idiopathic. [196] Hospital Episode Statistics in the UK and similar data from the USA suggest that men are affected with an increasing incidence from about 10 in every 100,000 up to 25 years, to 40 in every 100,000 by the age of 65 years, and > 100 in every 100,000 over 65 years. [198, 199]
However, while female urethral strictures (FUS) are not so common, they can lead to equally irritative and obstructive voiding symptoms. [200]. Female urethral strictures affect 0.1–1% of women with voiding complaints. In a review by Chakraborty et al. of surgical interventions for female urethral strictures, 53.48% were presumably idiopathic and 91.29% had a history of prior intervention. [201] Smith et al. found 8% of strictures in females were a result of inflammation and infection and 6.6% of trauma. [11]
Urethral strictures can occur at any point along the urethra in males, but are commonest in the bulbar urethra (50 %) and at the urethral meatus. Intermittent dilatation is a well-established method of palliative management of refractory urethral strictures in selected patients as it can reduce stricture recurrence up to 68%. Urinary diversion (e.g., continent stoma or ileal conduit) is required in patients when urethral reconstruction is not possible, or after failed attempts at repair. [202, 203]
A Cochrane review [204] concludes that there are insufficient data to determine if urethral dilatation, endoscopic urethrotomy, or urethroplasty is the best intervention for urethral stricture disease in terms of balancing efficacy, adverse effects and costs. A small RCT (n=49) comparing clean intermittent self-catheterisation (CISC) and repeated sounds dilatation showed a statistical significant difference for patients performing CISC who had a significant improvement in flow rate and improved QoL. [205]
Why
Intermittent urethral dilatation is performed to maintain the patency of the urethra, bladder neck, or external urethral meatus. The decision to commence urethral dilatation is on medical advice. Long-term IC in women who have strictures can avoid major surgery.
When
When the medical decision is made that a patient would benefit from urethral dilatation, the patient is taught to self-dilate within a month of surgery. Ideally, the catheter should be a size 16 or 18 Ch. [202] Occasionally, the patient may need to commence intermittent self-dilatation (ISD) initially with a smaller Charrière size because the urethra does not accommodate a larger catheter. If this is the case, the Charrière size should be increased over time to a larger diameter catheter if possible.
How long
Urethral dilatation is considered a long-term solution; patients should be informed that they need to continue to dilate intermittently in the long term [12], unless reconstructive surgery is considered.
15.3 Materials and procedure
The procedure and material for intermittent urethral dilatation are the same as for IC.
When teaching patients to self-dilate, it is important that healthcare professionals and patients are aware of the location of the urethral stricture. This determines how far the catheter needs to be inserted along the urethra because all strictures require the catheter to be advanced beyond the stricture.
Female patients:
In practical terms, because of the shortness of the female urethra, women should introduce the catheter all the way into the bladder to ensure the stricture has been passed.
If a woman has difficulties to see the location of the urethra, a mirror can be helpful (details in Appendix F).
Male patients:
- Meatal strictures and strictures occurring in the penile urethra can be negotiated with a meatal dilator or a female-length catheter.
A male-length catheter is required for all other urethral strictures.
- Mid-penile strictures need to be passed beyond the stricture. If there is any doubt that the stricture has been negotiated, the catheter should be passed into the bladder.
- For all bulbar and membranous strictures, the catheter should be advanced all the way into the bladder to ensure that the stricture has been dilated.
The procedure for undertaking urethral dilatation is found in:
Appendix F: Intermittent urethral dilatation – female and male
The principles for teaching urethral dilatation are the same as for teaching patients and caregivers how to catheterise intermittently.
| Recommendations | LE | GR |
| Adhere to the hospital protocol on the frequency of dilatation | 4 | C |
| Advise a catheter type suitable for the location of the stricture | 4 | C |
15.4 Frequency of dilatation
The frequency of dilatation is prescribed by a medical doctor or nurse specialist (depending on local policy). In the early days of learning, frequency should be up to daily. Thereafter, frequency can be less often depending on individual symptoms. [11, 12, 202] The recurrence of strictures is much lower when urethral dilatation is continued for > 12 months. [205]
