5. TERMINOLOGY (DEFINITIONS)
4.1 Urethral intermittent catheterisation
Intermittent (in/out) catheterisation (IC) is defined as drainage or aspiration of the bladder or a urinary reservoir with subsequent removal of the catheter. [8]
For sterile, aseptic, non-touch and clean techniques, the Working Group decided to use the definitions below, because the definitions in the literature were not coherent.
4.2 Catheterisation techniques
There are various IC techniques, but unfortunately, it is not always clear what is exactly meant by a particular technique that is mentioned in the literature. Also, practice differs even though the same name may be used. The techniques mentioned in these guidelines are defined outlined below.
Sterile technique
Complete sterile technique is only used in operating theatres, diagnostic situations, and immunocompromised patients. Sterile technique implies that all the material is sterile and catheterisation is performed with sterile gown, gloves, etc. – that is, full operating theatre conditions.
It is now widely accepted that sterile intermittent catheterisation (SIC) has been used incorrectly for aseptic technique.
The focus in these guidelines is on aseptic technique, which is the most commonly used technique in different settings.
Aseptic technique (When aseptic technique is mentioned in these guidelines, it refers to this definition)
- Use of a sterile catheter
- Cleansing of the genitals (water and soap)
- Use of sterile gloves
- Use of sterile lubricant (if the catheter is not pre-lubricated)
- Use of sterile tweezers (optional)
Non-touch technique
A non-touch technique is an aseptic technique that is usually performed with a sterile ready-to-use catheter.
An insertion grip/sleeve or special packages can be used to touch the catheter. [9] Additionally, limiting touch to only the conus side of the catheter is also considered a non-touch technique.
- Cleansing of the hands
- Non-sterile gloves
- Cleansing of the genitals (water and soap)
- Use of a sterile or ready-to-use catheter
Clean technique
Clean technique is only used by patients or caretakers in the home setting.
- Use of a sterile catheter
- Cleansing of the hands
- Cleansing of the genitals (water and soap)
- Use of non-sterile or sterile lubricant (if the catheter is not pre-lubricated)
Hygienic technique
The term hygienic technique is sometimes used for aseptic and sometimes for clean technique. The Working Group decided not to use this term.
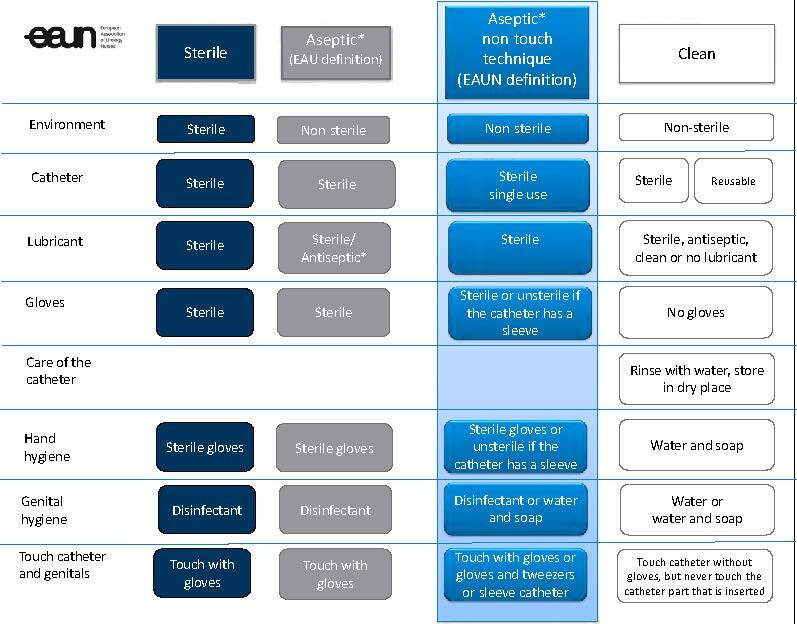
Diagram 2. Details of different IC techniques
4.3 Further definitions
Urethral stricture/stenosis
Urethral stricture is the preferred term for any abnormal narrowing of the anterior urethra, [10] which can lead to various urinary symptoms and complications. Urethral strictures are either a single or multiple narrowings along the length of the urethra and are more common in men than in women. [11-13] In men, urethral stricture refers to a narrowed segment of the anterior urethra due to fibrosis and cicatrisation of the urethral mucosa and surrounding spongiosus tissue (“spongiofibrosis”). [14, 15] In the male posterior urethra, there is no spongiosus tissue and at this location, the term stenosis is preferred. [14, 15].
There is no universal definition for what constitutes a female urethral stricture (FUS). It is defined by most authors as a fixed anatomical narrowing causing reduced urethral calibre, [11, 16] variously defined as between < 10 Fr to < 20 Fr [17, 18] with the majority defining < 14 Fr as diagnostic, compared with a normal urethral calibre of 18-30 Fr.
In transgender patients, the term stricture is also used to define a narrowing of the reconstructed urethra despite the absence of surrounding spongiosus tissue.
Urethral meatal stenosis
Narrowing of the distal opening of the urethra that may be congenital or occur secondary to infection, inflammation, or as a result of surgical (open or endoscopic) intervention. [19]
Bladder neck stenosis
Abnormal narrowing of the bladder neck, mostly related to previous surgery.
Dilatation
Dilatation refers to the condition of an anatomical structure being dilated beyond its current dimensions.
Urethral dilatation refers to stretching the stenotic part of the urethra with semi-rigid, rigid dilators or balloon distention to treat abnormal narrowing and temporarily improve voiding.
For the purpose of this document IC is deemed to include both urethral IC and urethral intermittent dilatation.
Healthcare-associated infections (HCAIs)
Healthcare-associated infections occur while receiving health care, or develop in a hospital or other healthcare facility, that first appear ≥ 48 h after hospital admission, or within 30 days after receiving health care. [20]
Haematuria
There are two kinds of haematuria. Microscopic haematuria as three or more red blood cells per high-power field (RBC/HPF) on urine microscopy. [21] and macrohaematuria (also called gross or frank haematuria) which is visible with the naked eye from a concentration as low as 1 ml blood per litre of urine. [22]
Urinary retention
Urinary retention is when the bladder does not empty completely or at all. Acute urinary retention is defined as a painful, palpable or percussable bladder, when the patient is unable to pass urine. [8]
Chronic urinary retention is defined as a non-painful bladder that remains palpable or percussable after the patient has passed urine. Such patients may be incontinent. [8]
Post-void residual (PVR)
Post-void residual is defined as the volume of urine left in the bladder at the end of micturition. [8]
Bacteriuria
Bacteriuria is the presence of bacteria in the urine and it can be classified as asymptomatic or symptomatic bacteriuria. For a urine specimen collected by in and out catheter, a count of > 100 colony-forming units (CFU)/ml is consistent with bacteriuria. [23]
Symptomatic bacteriuria is defined as a significant number of bacteria in the urine that occurs together with urinary tract symptoms such as dysuria and fever.
Asymptomatic bacteriuria is defined as a positive urine culture but with absence of symptoms. [24]
Urinary tract infection (UTI)
A urinary tract infection (UTI) is an infection involving any part of the urinary system, including urethra, bladder, ureters, and kidney.
UTI is defined as bacteriuria or funguria together with urinary tract symptoms such as dysuria and fever with a count of > 103 CFU/ml.
The definition of CAUTI belongs to indwelling catheters and is not applicable for IC. [25]
Table 3. Classification of UTI
| Classification of UTI | |
| Uncomplicated UTIs | Acute, sporadic or recurrent lower (uncomplicated cystitis) and/or upper (uncomplicated pyelonephritis) UTI, limited to non-pregnant women with no known relevant anatomical and functional abnormalities within the urinary tract or comorbidities. |
| Complicated UTIs | All UTIs which are not defined as uncomplicated. Meaning in a narrower sense UTIs in a patient with an increased chance of a complicated course: i.e. all men, pregnant women, patients with relevant anatomical or functional abnormalities of the urinary tract, indwelling urinary catheters, renal diseases, and/or with other concomitant immunocompromising diseases for example, diabetes. |
| Recurrent UTIs | Recurrences of uncomplicated and/or complicated UTIs, with a frequency of at least three UTIs/year or two UTIs in the last six months. |
| Urosepsis | Urosepsis is defined as life threatening organ dysfunction caused by a dysregulated host response to infection originating from the urinary tract and/or male genital organs. |
[23]
However, different organisations use different definitions as shown in Table 4 (differences in italic font).
Table 4. Differences in definition of UTI
| Source | Signs/symptoms | Lab parameters | Differences | |
| Blok et al. EAU Guidelines on Neuro-Urology. Arnhem: European Association of Urology; 2022 | Fever Incontinence Spasticity Lethargy Cloudy urine | Malodorous urine Kidney/bladder pain Dysuria Autonomic dysreflexia | 102 CFU/ml | Laboratory parameters |
| Hooton et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Clin Infect Dis. 2010 | Fever Rigors Altered mental status Lethargy | Flank pain Acute haematuria Dysuria Urgent urination | 103 CFU/ml | No other identified source of infection, altered mental status, haematuria, urgency |
| Goetz et al. International Spinal Cord Injury Urinary Tract Infection Basic Data Set. Spinal Cord. 2013 | Fever Incontinence Spasticity Lethargy Cloudy/malodorous urine | Pyuria/leukocyturia Kidney/bladder pain Dysuria Autonomic dysreflexia | 103 CFU/ml | New onset of symptoms, pyuria |
From: UTI-assessment tool presentation by Dr. A. Krassioukov, Canada
[26-28]
